AMR: “A little less conversation, a little more action, please”
Hello there! I’m Carolyne Horner, the newly appointed Scientific Lead at Una Health Ltd. This month, I have been asked to write about the wider issues of antimicrobial resistance, also known as AMR.
Goodness me, where to begin?!
The benefits of using antimicrobial drugs in human and animal health for treating infection are well-known; however, using these drugs are not without challenges, the development and spread of microorganisms (or bugs) that are resistant to these drugs being one major challenge.
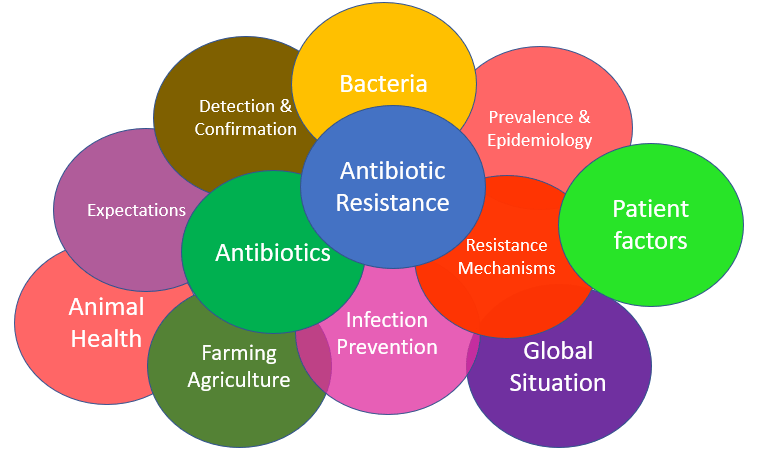
Antimicrobial resistance is a complex, multiple layered, interlinking concept (Figure 1). Accordingly, there are many sources of information, reports, websites, blog posts about the subject. Finding relevant, accurate and up-to-date information can be a challenge. One intention of this post is to signpost the reader to recent reading/resources.
Each one of the topics shown in Figure 1 would fit into the category of ‘wider issues of antimicrobial resistance’; however, for this post, I’ve chosen to talk about three of my favourite ‘soap box’ topics: awareness, accountability, and translation. The scope of each of these three subjects is broad and much has been written/debated about each one.
But, in the words of Elvis, I propose “A little less conversation, a little more action, please” (which was also used in an AMR blog post by Brendan Shaw, so I am in good company!)
Wider Issue 1: Awareness
What does AMR mean to you?
Active metabolic rate? Analytical Measurement Range? Average Message Rate? Automatic Meter Reading? Advanced Market Research? American Medical Response?
In healthcare, AMR stands for Antimicrobial Resistance.
Antimicrobial or antibiotic? Antimicrobial is an all-encompassing term that includes drugs that treat infections caused by different microorganisms: bacteria (antibiotic), fungi (antifungal), parasites (antiparasitic) and viruses (antiviral). Anti-infective, antibacterial, drug-resistant are other terms that may be used.
And who or what is resistant?
Myth: Antimicrobial resistance means that the human body has become resistant/immune to the antimicrobial drug and that is why the drug doesn’t work anymore.
Fact: Antimicrobial resistance is when bacteria that are causing an infection in the body have developed ways to stop the antimicrobial from entering the bacterial cells. The drug no longer kills the bacteria and the infection remains untreated.
In June 2015, Wellcome published a report “Exploring the consumer perspective on antimicrobial resistance”, which investigated the knowledge, attitudes and perceptions of the public on antimicrobial use and antimicrobial resistance. They found that the three-letter acronym ‘AMR’ ‘meant nothing’ to participants.
Since then, Wellcome has been working hard to reframe antimicrobial resistance. In November 2020, they published “Wellcome Monitor 2020: Public perception of drug-resistant infections” and reported that 81% of the people surveyed had come across the term ‘drug-resistant infection’ and had an understanding of what the term meant.
AMR or drug-resistant infection? It’s not difficult to work out which term is easier to understand.
What is needed to raise awareness?
A common language and terminology that is easy to understand
Dr Eva Krockow from the University of Leicester has written an insightful article where she proposes that antimicrobial resistance needs to be renamed. Dr Krockow sums up the problem succinctly: “The current name is inconsistently used, difficult to pronounce and lacks meaning for lay audiences. It also fails to express the magnitude of the phenomenon’s potential consequences for human medicine.”
Wellcome have produced a practical toolkit “Reframing resistance – How to communicate about antimicrobial resistance effectively” centred around five principles:
- frame antimicrobial resistance as undermining modern medicine
- explain the fundamentals succinctly
- emphasise that this is a universal issue; it affects everyone, including you
- focus on the here and now, and
- encourage immediate action
A common logo
In November 2019, the Joint Action on Antimicrobial Resistance and Healthcare Associated Infections (EU-JAMRAI) launched a contest to find the first global symbol of Antibiotic Resistance awareness (think red ribbon for HIV awareness). The winning symbol designed by David Ljungberg, Sweden, is ingenious (see Figure 2) and captures many aspects of AMR.
The language used to describe AMR matters if people are going to change their behaviour towards the use of antimicrobials and contribute to the reduction in development of resistance, at whatever level.

The Joint Action on Antimicrobial Resistance and Healthcare Associated Infections (EU-JAMRAI)
Wider Issue 2: Accountability
AMR is a global health concern
Bugs don’t respect international boundaries; drug-resistant bacteria in one country could quickly spread to become prevalent in other countries. Who is responsible for monitoring this spread? Who is responsible for preventing any further spread?
Different countries have different AMR priorities according to the prevalence of disease in that location [think drug-resistant tuberculosis (bacteria), drug-resistant malaria (parasite), drug-resistant HIV (virus) where prevalence is higher in certain regions] but resistance to antibiotics is seen as the most urgent drug resistant trend.
In May 2015, the World Health Assembly [the decision-making body of the World Health Organisation (WHO)] endorsed a global action plan to tackle antimicrobial resistance and urged all Member States to develop and have in place a National AMR Action plan by 2017. The UK have a 5-year AMR action plan and a 20-year AMR vision.
Governmental Accountability
In the UK, All-Party Parliamentary Groups (APPGs) are groups made up of MPs and Members of the House of Lords from across all political parties that meet to discuss topics of particular interest. While APPGs don’t have any formal standing in parliament, they serve to bring interested parties together to raise concerns and discuss possible actions.
In September 2020, the APPG on Antibiotics, wrote a letter to the government about the possibility of appointing a UK Government Minister who would have the authority to address drug-resistant infections and pandemic prevention and preparedness.
Having an accountable UK Government Minister would ensure that AMR is on the UK’s political agenda all of the time, driving change in policy.
Wider Issue 3: Translation
Advances in our understanding of AMR are being made all the time, with a constant stream of publications, and research outputs; however, there seems to a hurdle of translating the science into clinical practice and thus into patient-centred care. These hurdles apply to changing behaviours towards the use of antimicrobials, using antimicrobials appropriately, or introducing rapid diagnostic kits into primary care.
Using antimicrobials appropriately
Using antimicrobials appropriately, also known as antimicrobial stewardship (or AMS, another three-letter acronym!), is a strategy that can be applied to human healthcare but is also applicable to other settings where antimicrobials are used (veterinary medicine, agriculture, and environmental settings).
The subject of antimicrobial stewardship is too vast to explore in this post so for now, I’ll point you to a review by O.J Dyer and colleagues from the ESGAP (ESCMID Study Group for Antimicrobial stewardshiP) and to a diagram of the core elements of AMS from the Global Alliance for Infections in Surgery.
Through a multidisciplinary team, successful AMS programmes translate high quality evidence into clinical practice and are a driver for improvements in patient care.
Diagnostic stewardship
Similarly, diagnostic stewardship (is DS the right acronym?!) is a concept that encompasses using “the right test, on the right patient at right time” (see a review by Kevin Messacar and colleagues). Diagnostic stewardship principles aim to lead to appropriate treatment, resulting in a better patient outcome, and appropriate infection prevention interventions, thereby reducing the risk of transmission of infection.
While “the right test, on the right patient at right time” may seem obvious, it is important to determine the impact of diagnostic testing in any particular care pathway. For instance, rapidly available bacterial identification may not necessarily translate into changes in patient care (see the results of one intervention published by Alasdair MacGowan and colleagues).
But, to return to Elvis; enough talk/words, what about actions?
What can you do?
Become an advocate for change
It is within our gift to leave future generations with hope that antimicrobial drugs will still work for their lifetime and beyond. We all have a role to play in securing the future of antimicrobial drugs.
Don’t know where to start?
Dame Sally Davis, UK Special Envoy on Antimicrobial Resistance, recently wrote on the News and Views pages of the British Society for Antimicrobial Chemotherapy (BSAC) that many people do not know what they can do about AMR. As discussed earlier in this post, it’s easy to see why taking action against AMR seems daunting.
- Number one action – Wash your hands! Properly! No excuses!
- Aside from handwashing, there are many campaigns to raise awareness of AMR. Here are links to two pledge-based UK campaigns: Antibiotic Guardian and Seriously Resistant. Sign up, choose a pledge and use the resources available to educate your nearest and dearest.
- For more ideas, James Redfern and colleagues summarise public engagement activities that have been used to raise awareness of antimicrobial resistance among the general public in the UK
- Every year, 18-24 November marks World Antibiotic Awareness Week (WAAW). Lots of AMR awareness raising activities take place during this week, with many educational resources becoming available.
- Still want more? See the blog written by Tommy Bullen at the London School of Hygiene and Tropical Medicine for another ‘Five things you didn’t know about Antimicrobial Resistance (AMR)’.
Una Health want to hear from you. What are your thoughts on AMR? What are your ‘soap box’ AMR topics? What actions would you like to see? What are your experiences of AMR? What should antimicrobial resistance be renamed as? What can Una Health do for you?