“If, when, why, what?”: The principles of diagnostic stewardship according to The Pet Shop Boys
Publication Date: 30 September 2021
Hello there!
This month I explain the role of diagnostic stewardship in the fight against antimicrobial resistance (AMR) (see here for the first Una post about AMR). I’ll begin by explaining the principles of diagnostic stewardship, discuss why diagnostic stewardship is important, and end with a summary about what diagnostic stewardship means for antibiotic prescribing and patient care.
Something old, something new
Considering that the technique of looking for microbes down a microscope is around 350 years old, diagnostic stewardship is a relatively new concept to be applied to microbiology.
Stewardship may be defined as “the job of supervising, managing or taking care of something”; therefore, my interpretation of diagnostic stewardship would be ‘taking care of’ antibiotics by ‘supervising the use of diagnostic tests’, i.e., by making sure that diagnostic tests in microbiology are used appropriately.
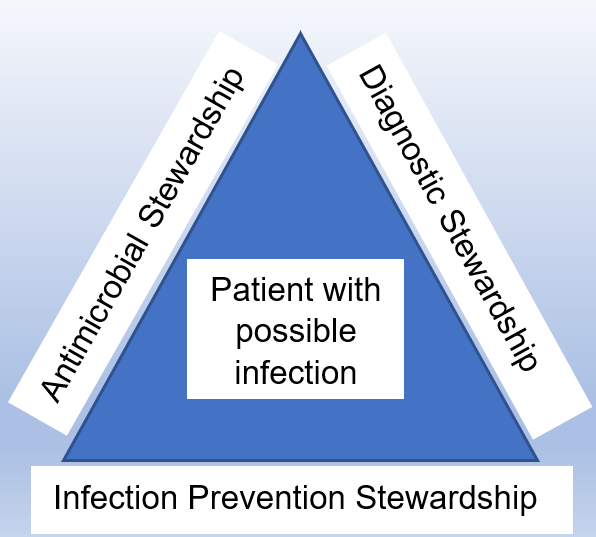
Dik et al. (2015) perhaps were one of the first to use the term diagnostic stewardship in the way that we think of it today when they proposed a trio of interlinking stewardship programmes: 1) diagnostic, 2) antimicrobial, and 3) infection prevention, as a multidisciplinary approach to the management of a patient with an infection (Figure 1).
Right test, Right patient, Right time
Here is one definition of diagnostic stewardship from Messacar et al., 2017:
“The goal of diagnostic stewardship is to select the right test for the right patient, generating accurate, clinically relevant results at the right time to optimally influence clinical care and to conserve health care resources.”
I also like the following definition:
“Supporting the practice of robust microbiological diagnosis in patients presenting with clinical symptoms.”
This definition reminds us that it may not be appropriate to take a urine sample for microbiological investigation from a young, fit and healthy patient with a broken leg who has no symptoms of a urine infection, just because urine is an easy sample to collect.
But what is the significance of The Pet Shop Boys?
By now you may be wondering what The Pet Shop Boys have to do with diagnostic stewardship and it’s a good question!

https://www.popexpresso.com/2020/12/19/pet-shop-boys-version-always-mind-no-1-day-1987/
If you are of a certain age and grew up in the 1980s, you may recall a song by The Pet Shop Boys: West End Girls. In the song are the lyrics….
“If, when, why, what?
How much have you got?”
As I was preparing this post, it occurred to me that these are questions that may be applied to diagnostic stewardship:
- If? – do you need to test?
- When? – are you going to take a sample and request a test?
- Why? – are you requesting the test?
- What? – are you going to test; what are you going to do with the results?
- How much have you got? – how much funding do you have to pay for testing?
Even if you don’t know the song, it’s a catchy way to remember the key diagnostic stewardship principles!
The importance of getting it right first time
Morjaria and Chapin (2020) describe a case of a patient with a life-limiting malignancy who endured overzealous diagnostic test requests and the impact that this had for the patient and family.
Some simple thoughts:
- Time is precious
- Resources are limited
- Diagnostic tests cost money
- Prescribing a course of antibiotics may be easy, quicker to achieve, and cheaper than completing a diagnostic test but is this the right approach?
For these reasons (and more), it is important that, to the best of our ability, we get the diagnosis right first time in patients with an infection.
| Concept | Consideration | Benefit |
| Right Patient | Inappropriate testing can cause harm and may lead to medical errors Does the patient have the clinical signs and symptoms of an infection? Will the result of the test influence patient care? | Patient dignity Patient safety – decreased risk of adverse events from over sampling (i.e., think lumbar puncture, venous blood) Patient convenience |
| Right Test | Do you need to test? What do the guidelines/algorithms recommend? Will you request a point-of-care test or a laboratory test? What are the performance characteristics of the tests that are available? Is a rapid test required? Is culture required to determine antimicrobial susceptibility or for surveillance purposes? | Faster turnaround of results from a laboratory not being burdened by unnecessary testing Better use of available resources Capacity to develop and improve services Efficient workflow |
| Right Time | How long does it take to get a result? Time to get the sample to the laboratory (don’t miss the transport!) Urgent testing or batch testing 24/7 or 9-5 testing availability | Informed clinical decision making Increased diagnostic certainty |
| Right Interpretation | Have the results been reported correctly? Have the results been interpreted correctly? How easy are the results to interpret by the end user? Selective reporting of the antibiotics released on a susceptibility testing report | Selective reporting can help improve antibiotic use by reducing both unnecessary and inappropriate prescribing |
| Right Action | Reduce inappropriate antibiotic prescribing Review antibiotics and take action (Stop, change or continue) Implement infection control/public health interventions | Optimal therapy for the patient Decrease antimicrobial resistance Decrease transmission of infection to others |
What difference does diagnostic stewardship make?
There are many published examples of diagnostic stewardship interventions (actions) that have resulted in reduced antibiotic prescribing and/or reduction in laboratory workload (Table 2 lists a small selection).
Diagnostic stewardship interventions are often described as part of a quality improvement programme or may be reported as part of an antimicrobial stewardship intervention.
| Sample type | Action | Impact on antibiotic prescribing/other |
| Wound swabs | Rejection of low-quality wound swabs | Antibiotic prescriptions reduced. Resource savings for the microbiology laboratory: decreased workload and use of reagents |
| Urine samples | Restriction of urine culture to patients with genuine urinary tract infection (UTI) | Antibiotic prescriptions reduced. Not prescribing antibiotics had no effect on patient mortality. No patients with unreported urine culture developed bacteraemia from untreated UTI |
| Urine samples | Practitioners required to choose an indication for urine culture | 40% reduction of urine cultures ordered 15% reduction in days of antibiotic therapy Yearly savings >$500,000 |
| Blood cultures | Clinical decision-making tool regarding indications for taking appropriate blood cultures | Unnecessary blood cultures effectively and safely reduced |
Treat the patient, not the laboratory result
Accurate and timely microbiological diagnosis facilitates appropriate and timely antimicrobial prescribing and infection prevention interventions; however, there is no substitute for the human aspects of clinical care.
Diagnostic stewardship is an integral part of a much wider stewardship programme and requires a multidisciplinary approach with input from colleagues in the laboratory, microbiology/infectious disease colleagues, pharmacists, patient-facing clinicians and nurses, infection prevention colleagues. These healthcare professions all contribute skills and experience to clinical assessment, interpretation of results, and antibiotic prescribing, ultimately improving patient care.
Next steps
Here are some suggestions to improve your diagnostic stewardship practices:
- Think Pet Shop Boys: If, when, why, what, how much have you got?
- Educate – many patients (and healthcare professionals!) do not know what happens to a sample once it has been taken. Take this a great opportunity to raise awareness of the ‘hidden’ profession of pathology (The IBMS has a great resource: Do you know what happens to your sample?).
- Audit – identify areas of best practice and celebrate and share these; identify areas for improvement and make changes so that they become areas of best practice.
- Use clinical guidelines and algorithms when they are available. After all, someone somewhere has gone to an awful lot of trouble to develop these evidence-based resources.
- Finally, remember that every action has consequences: inappropriate microbiological testing has consequences for a patient, as does inappropriate antimicrobial prescribing.
Resources
The following two articles are both excellent sources of information for those who would like to learn more about diagnostic stewardship:
- Claeys & Novel, 2020: Diagnostic Stewardship: Beyond Managing Bloodstream Infections
- Salinas et al., 2018: Laboratory test inappropriateness: lessons revisited and clarified in seven questions
There is also an excellent (and free!) e-learning course from the London School of Hygiene and Tropical Medicine on the FutureLearn platform: The Role of Diagnostics in the Antimicrobial Resistance Response
Call to action
Una Health invite you to share any comments about your experiences of improving diagnostic stewardship by reducing inappropriate testing or introducing selective reporting. What song lyrics remind you of work-related themes?!