AMR awareness week 2023: Diagnostics as the Key to Antibiotic Stewardship
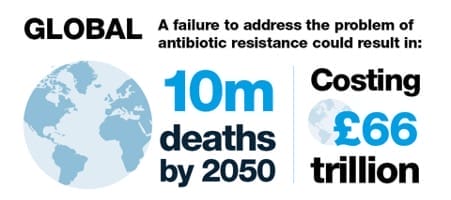
The urgency to tackle antimicrobial resistance (AMR) has never been more critical, as evidenced by the escalating toll of 1.2 million deaths attributed to resistant infections annually—a number steadily on the rise.
Current projections indicate a grim trajectory, with an anticipated increase to 10 million deaths by 2050 if effective measures are not promptly implemented. Swift and comprehensive actions to address AMR are imperative to avert this impending public health crisis.1
Rising Antibiotic Use Post-Pandemic
Following the pandemic, there has been a resurgence and rise of priority pathogen infections and antibiotic use has risen by 8.4% in 2022 versus 2021, the first increase since 2014 with primary care settings accounting for 80% of all antibiotics prescribed. This increase highlights the need for improvements towards the National Action Plan of reducing antimicrobial use by 15% by 2024 from a 2014 baseline.3
Deaths and Challenges in Antibiotic Resistance
In 2022, the estimated deaths due to antibiotic resistant infections was 2202, with AMR highest in deprived areas.3 The need for investment in the antibiotic pipeline is clearly recognised, with lack of R&D from large companies and no new classes of antibiotics coming to market since the 1980s as a result.
The Role of Diagnostics
While addressing the antibiotic pipeline is crucial, diagnostics play an equally – if not more- important role in the fight against AMR. Without the use of diagnostics, antibiotics are being used blindly, prescribed and used for infections (or non-infections) that may not warrant them. Differentiating between bacterial and viral infections is an obvious tool that could help ensure antibiotics are only used when actually needed. A diagnostic test that is widely available and an indicator of infection severity, is C-reactive protein.
C-reactive protein (CRP) is a well-studied non-specific inflammatory marker and is generally higher in bacterial than viral infections. It can support clinical decision making, particularly in patients presenting with lower respiratory tract infection (LRTIs) whereby the majority of which are viral (70%). CRP is an indicator of severity and can be used to assess if patients would benefit from antibiotic treatment. Point of care devices are available for CRP testing with performance comparable to laboratory results, enabling clinicians to perform a quick fingerprick test and make a better informed decision in the same appointment. The use in primary care has been found to reduce prescribing up to 42%, supporting the positive impact diagnostic tools have in optimising antibiotic use.2
Maintaining current antimicrobial prescribing practices puts us at risk of regressing to a pre-Fleming era, where even minor injuries could prove fatal. To avert this, it is imperative to channel investments towards the development and integration of point of care diagnostics within our healthcare system. This shift will be pivotal in eliminating inappropriate prescribing and safeguarding the longevity of our available antimicrobial treatment options.
Resources and further reading
- Health matters: antimicrobial resistance – GOV.UK (www.gov.uk)
- Frontiers | Guidance on C-reactive protein point-of-care testing and complementary strategies to improve antibiotic prescribing for adults with lower respiratory tract infections in primary care (frontiersin.org)
- English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) report 2023 to 2023 (publishing.service.gov.uk)

Discover QuikRead go® for CRP testing
QuikRead go is a reliable and rapid point of care analyser for CRP testing. Empowering informed decisions, it plays a crucial role in sustainable antibiotic use and supports effective antimicrobial stewardship.